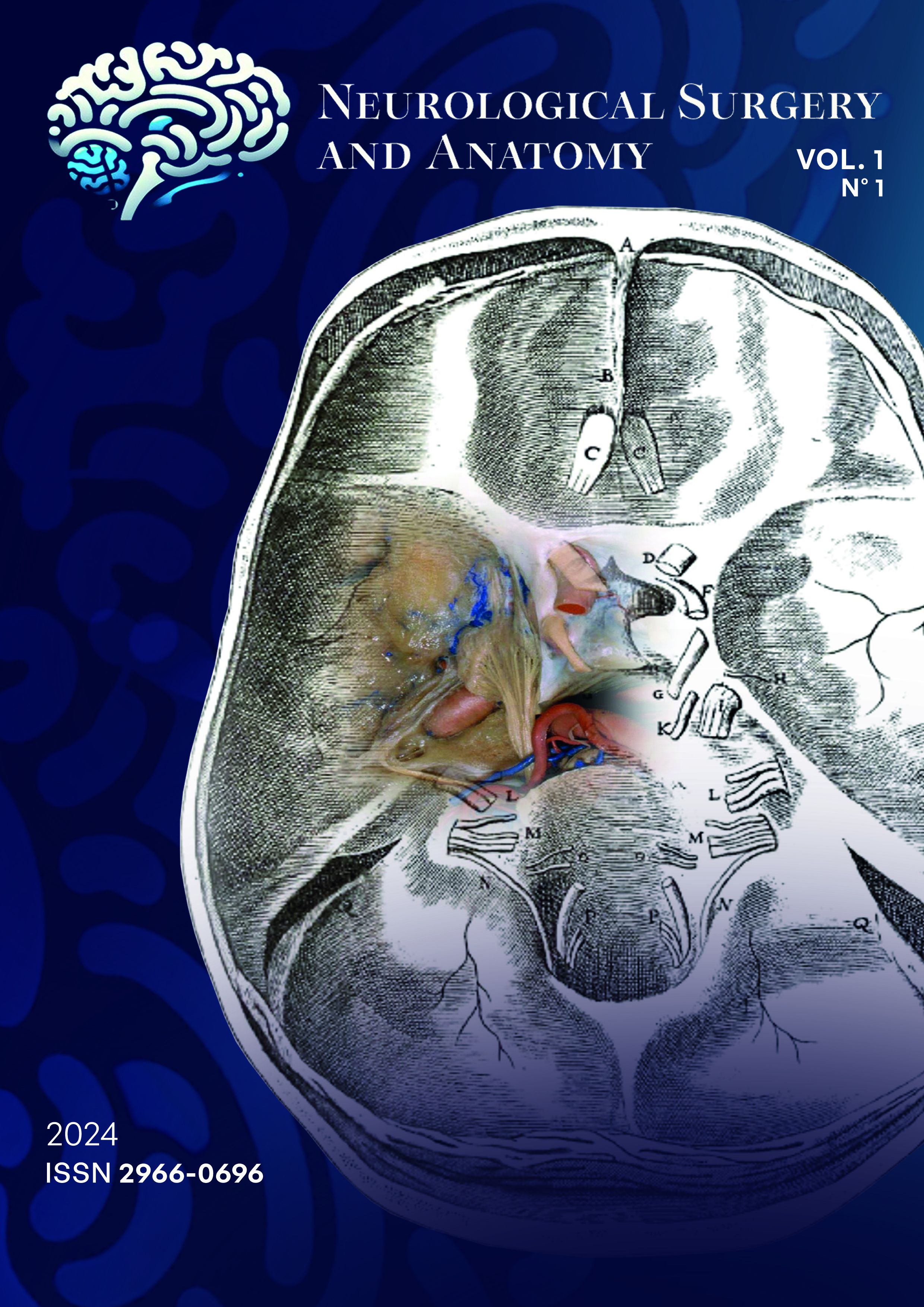
Exploring the third ventricular floor anatomy: clinical insights for endoscopic third ventriculostomy
Views: 261DOI:
https://doi.org/10.37085/nsa.2024.5Keywords:
Third ventricle, Basal cisterns, Third ventriculocisternostomy, Neuroendoscopy, Surgical anatomyAbstract
Introduction
Successful endoscopic third ventriculocisternostomy depends on understanding the third ventricle's floor and adjacent cisternal anatomical landmarks.
Objective
To explore the relationships among critical structures in this area to establish an anatomical classification for this region.
Methods
Sixty, silicone-injected, cadaveric heads were used. Measurements were taken at the level of third ventricular floor, cisterns, and tentorial edge, to classify the following: the size of the pre-mammillary area, suitable for third ventriculostomy; to determine whether the midbrain and optic chiasm are pre, normo or postfixed and to classify the size of the angle between the third nerves in the cistern.
Results
In this study, pre-mammillary area sizes were classified as small (12.5%), medium (62.5%), and large (25%). Midbrain positioning was prefixed in 19%, midrange in 57.1%, and postfixed in 23.8% of cases. Chiasm positioning showed 20% prefixed, 65% normofixed, and 15% postfixed. A significant inverse relationship emerged between the midbrain-dorsum distance and the angle between the third nerves at the peduncle (p=0.001). As the dorsum-midbrain distance increased, so did the distance from the dorsum to the basilar artery, basilar artery to the midbrain, and the size of the pre-mammillary area (p<0.001). A wider tentorial edge also correlated with a greater distance between the third nerves (p<0.05).
Conclusion
The midbrain's position significantly influences the safe space for third ventriculocisternostomy. A larger space is likely with a prefixed chiasm or postfixed midbrain. The midbrain position and tentorial notch width determine the lateral safety zone for a paramedian ventricular floor opening. Pre-operative assessment of these spatial relationships is useful.
References
Adler DE, Milhorat TH. The tentorial notch: anatomical variation, morphometric analysis, and classification in one hundred human autopsy cases. J Neurosurg 96: 1103-1112, 2002.
Correales M, Torrealba G. The third ventricle. Normal anatomy and changes in some pathological conditions. Neuroradiology, 11: 271-277, 1976.
Huber P, Rivoir R. The influence of intraventricular pressure on the size and shape of the anterior part of the third ventricle. Neuroradiology, 5:33-36, 1973.
Kier, EL: Comparative anatomy of the third ventricular region. In Apuzzo, MLJ: Surgery of the Third Ventricle, Williams and Wilkins, Baltimore, MD, 1987, 37-91.
Rhoton AL Jr. The lateral and third ventricles. Neurosurgery. 51(4, Suppl. 1): S1-207-S1-271, 2002.
Rhoton AL Jr. The sellar region. Neurosurgery. 51(4, Suppl. 1): S1-207-S1-271, 2002.
Rovira A, Capellades J, Grivé E, Poca, MA, Pedraza S, Sahuquillo J, Rodríguez-Baeza A. Spontaneous ventriculostomy: report of three cases revealed by flow-sensitive phase-contrast cine MRI. AJNR, 20: 1647-1652, 1999.
Schroeder HWS, Niendorf WF, Gaab MR. Complications of endoscopic third ventriculostomy. J Neurosurg 96:1032-1040, 2002.